Physical therapists: if you’re new to telehealth, you may not realize all the benefits remote therapy can offer you and your patients. In this post I provide a brief history of telehealth before sharing 3 telehealth trends that can help you improve patient care.
History of Telehealth
Telehealth has only recently become a household word, after seeing a 38-fold growth spurt since the Covid19 pandemic. But the concept of remote care has been around for decades, since the Civil War.
Physicians telegraphed medical scripts in the Civil War and telephoned diagnoses in the World Wars. By the 1960s, closed-circuit televisions allowed physicians to remotely monitor their hospital patients, while the moon landings spurred the telemetric transmission of biometric data.
At every turn, telehealth technology has evolved along with our communication technology, equipping health professionals with better ways to provide care.
Telehealth Today
PTs around the world got a crash course in telehealth at the onset of Covid19. We quickly learned that, when seeing a patient in person isn’t an option, telehealth technology can provide a digital platform to consult patients and demonstrate therapies.
Telehealth, or teletherapy in our case, is a real-time service, rendered by the use of a communication device such as a phone, tablet, or computer. Typically, both the patient and therapist use their device’s built-in camera and microphone to transmit audio and video feed over an internet connection.
It may sound simple, but telehealth technology is constantly evolving. Here are 3 trending ways PTs can utilize telehealth to improve their patient care.
3 Telehealth Trends
1. Virtual Appointments

The primary reason a therapist uses teletherapy is to keep virtual appointments with their patients. Instead of scheduling a patient in person, a clinic may offer a virtual option whereby the PT sees the patient remotely.
During the pandemic, virtual appointments helped keep many clinics afloat when many patients were sheltering at home and unwilling to be seen in person. But teletherapy is here to stay, because it offers many valuable benefits to the clinic and the patients.
Benefits of Virtual Appointments
One of the most salient benefits of telemedicine is the access it provides. It eliminates the barriers that arise from a patient’s lack of transportation or their discomfort with being out in public. It also gives the therapist a further reach in seeing patients who may otherwise live too far away for regular visits.
Compared to in-person meetings, telehealth visits tend to be timelier. They’re shorter and more punctual, without the likelihood of getting delayed by traffic. Virtual appointments are a snap to reschedule, so even if a patient cancels or doesn’t show, the therapist can easily move on to the next patient and keep the clinic running efficiently.
Disadvantages of Virtual Visits
Despite widespread support, teletherapy isn’t always an ideal option. There are a few major drawbacks to receiving treatment remotely; by its very nature it precludes the physical touch PTs use to assess, guide, and administer.
Therapists rely on their hands to test a patient’s muscle strength or assess their range of motion. But it’s impossible for a teletherapist to test for strength by manually resisting a specific movement. For this reason, therapists conducting a teletherapy visit must modify their strength and mobility tests, ideally by using a system that’s easy for even the least “tech-savvy” of their patients to understand.
On that point: even if a therapist is tech-savvy, it doesn’t mean their patients are. One big drawback to virtual appointments is the learning curve of video conferencing, which may distract a patient’s focus if they cannot easily manage the video setup.
2. Online Coaching and Accountability

A major perk of teletherapy is the accountability a therapist can provide in between visits. We call these check-in appointments—quick calls to monitor how well the patient is tolerating treatment and whether they are continuing their exercises at home.
A therapist with telehealth technology can provide online coaching in between appointments. This may involve having the patient demonstrate their home exercises in front of the camera so the therapist can verbally correct their form. The therapist may also use the camera to demonstrate new exercises or modifications that help the patient progress through their current HEP.
All told, online coaching can provide the encouragement and accountability a patient may need to continue making progress.
Benefits of Online Coaching
Online coaching benefits therapists in the same way virtual appointments can: it improves access and optimizes a clinic’s schedule. From a patient’s perspective, teletherapy is usually much more affordable than in-person visits. Insurance reimbursement rates tend to be lower for teletherapy, keeping costs down for patients.
But saving money doesn’t necessarily mean compromising on care. One study showed that telehealth visits helped patients recovering from a total knee replacement save $2700 on physical therapy at the 12-week mark. These TKA patients demonstrated equivalent outcomes and even lower re-hospitalization rates than their counterparts who had received in-person PT.
Limitations of Online Coaching
Although online teletherapy may work well for patients in some cases, it’s not for everyone. Therapists face several limitations in administering online coaching as opposed to in-person therapy.
For example, a teletherapist is at the mercy of their patient’s camera for viewing and monitoring their movements. Without constant instruction to move the camera, the therapist cannot catch all the angles of a patient’s movement, as they can by simply walking around the patient in the clinic.
Furthermore, without being there in person, a therapist cannot offer physical support in a guiding hand or stable stance for the patient as they perform new exercises. A patient with poor balance may risk falling at home without the supervising, in-person support of a therapist.
3. Remote Therapeutic Monitoring Codes

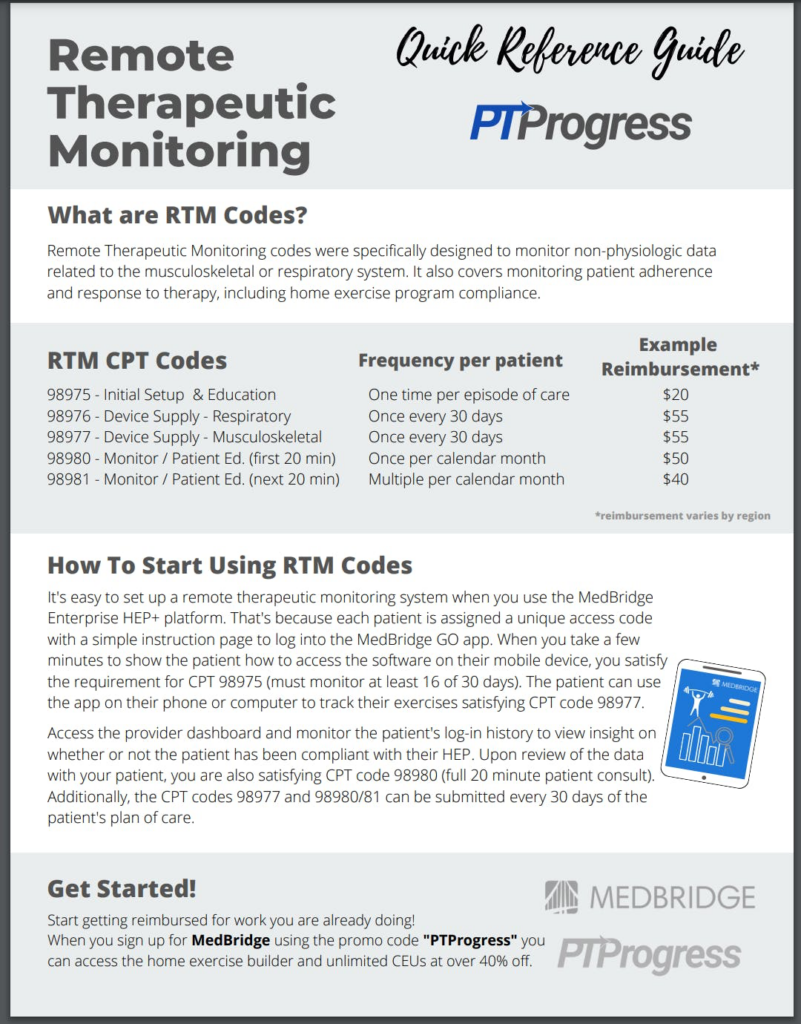
Conducting a virtual appointment or online coaching requires a therapist’s time, attention, and expertise. Luckily, therapists can now be fairly reimbursed for the work they do behind a computer, thanks to the 2022 release of 5 RTM codes.
RTM stands for Remote Therapeutic Monitoring, the work therapists perform remotely with their patients. These codes address the logistic side of telemedicine, putting dollars and cents to all therapeutic activity—even remote care—a PT administers.
How It Works
To qualify as RTM, the patient must use a medical device or qualifying mobile phone software to track and log non-physiological data. This data may include a record of the patient’s adherence to treatment or a chart of the patient’s heart rate or blood pressure levels while performing exercises. In addition to what’s automatically uploaded, the patient may also self-report less-perceptible data such as pain level or fatigue.
The therapist, meanwhile, monitors this activity and responds to it. Perhaps they’ll modify an exercise based on the patient’s feedback or schedule an online coaching to provide needed accountability. For the teletherapist, “out of sight” does not mean “out of mind,” and remote therapeutic monitoring can help them continue supporting their patients.
Reimbursing with RTM
RTM codes can provide worthwhile reimbursement for this non-clinical time. Even the process of setting up a patient with a medical device and teaching them how to use it can translate into billable reimbursement.
To learn more about the five RTM codes and their reimbursement rates, check out this article. Included is a quicksheet designed to help you learn and apply the RTM codes to your clinical practice.
Telehealth Trends: Summary
Now that social distancing restrictions have evaporated and the “new normal” has set in, it’s clear that telehealth is here to stay. These 3 telehealth trends can help you optimize your teletherapy visits so it benefits your patients—and you—as much as possible.
If you’re still unsure about telehealth, maybe a class or two can help you feel more comfortable. MedBridge offers several continuing education courses on telehealth technology as well as ethical considerations for home care technology. These courses may even apply towards your license renewal, doubling your efforts to improve patient care as you advance your own career.