If you ever have the misfortune of going to the ER, you’ll probably be asked to rate your pain on the Universal Pain Scale. It’s not just for posterity; pain assessment helps medical professionals ensure a proper diagnosis, administer appropriate treatment, and keep you comfortable under their care.
Medical facilities all over the world use some form of a pain scale. The simplest pain scales use a single continuous line to measure pain intensity, while more elaborate scales may combine several points of data. Despite this wide range of pain scales, one stands out from the rest: the Universal Pain Scale or Universal Pain Assessment Tool (UPAT).
What is the Universal Pain Scale?
The Universal Pain Scale measures a patient’s pain in three ways. First, it displays a range of facial expressions, from smiling to crying, to reflect the pain experience. Above the lineup of faces is a numerical rating scale ranging from 0 to 10, which patients may use to pinpoint the severity of their pain. In addition, the UPAT provides an array of tolerance indications to further elaborate on the pain—that it “interferes with tasks” or “requires bedrest,” for example.
Let’s take a look at the three components of the UPAT one by one.
The FACES® of the Universal Pain Scale
The famous 6 expressions on the UPAT come from the Wong-Baker FACES® scale, the brainchild of two pediatricians working in the 1983. Wong and Baker wanted a scale that was concise, easy to use, and most importantly, effective at getting patients the treatment they needed.
To develop the scale, Wong and Baker asked 50 children in their hospital’s pediatric and burn units to draw faces illustrating a variety of pain levels they’d experienced. The researchers then collected the most frequently drawn features and created 6 standard facial expressions out of the composites of those features. They gave these redrawn faces to a new set of children, who readily understood the depictions.
Not only was the FACES® scale universally accepted by other children, it successfully helped the children communicate their perception of pain. Decades of research and validity testing proves that the Wong-Baker FACES® scale is one of the most intuitive scales for patients of all demographics—including age, cognitive ability, and nationality.
Numerical Rating Scale
The faces of the Universal Pain Scale accompany two iterations of a numerical rating scale. One is free-standing at the top of the chart. The other scale clarifies and clumps together the facial expressions into 4 categories: no pain, mild pain, moderate pain, and severe pain.
In the UPAT, 0 corresponds to no pain at all, while mild pain belongs to numbers 1 and 2. Moderate pain registers as 3-6 on the scale, and the rest of the scale from 7-10 reflects severe pain. For simplicity, a physician may ask you to use the first numerical rating scale and rank your pain from 0 to 10, with 0 being no discomfort and 10 being the most intolerable pain ever.
Activity Tolerance Scale
In the UPAT, patients can compare a numerical rating or facial expression with other indications that coincide with that level of pain. For example, a patient experiencing moderate pain of level 6 may agree that it’s interfered with concentration. Despite selecting a neutral-looking face, a patient with a pain level of 3 or 4 may admit that their discomfort is becoming difficult to ignore.
Some versions of the UPAT include behavioral indications, such as “holds breath” or “furrows brow” to characterize each point along the scale. Altogether, the UPAT uses both broad imagery and specific language to help patients communicate their pain in a way providers can understand.
Other Pain Scales
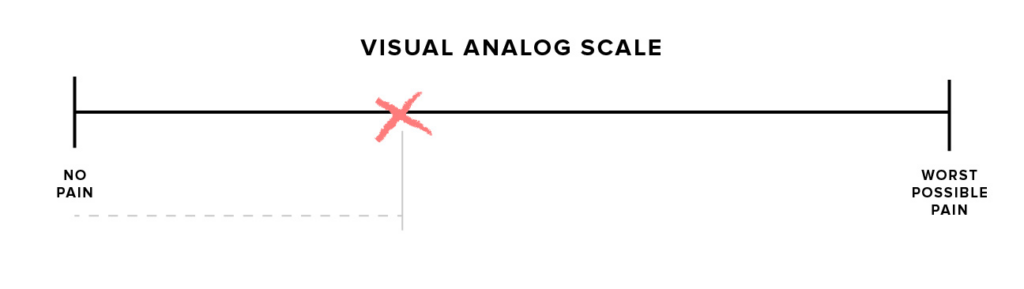
Although the Universal Pain Scale is the most common type of pain assessment tool, it isn’t always the best one for every case. Some scales are more basic, such as the visual analog scale, which is essentially a continuous line between a point of No Pain and a point of Worst Possible Pain. To use the scale, a patient simply marks an “x” along the line.
Other pain scales are extremely intricate, evaluating a patient’s quantitative and qualitative data to assess their pain. For example, the FLACC scale measures the Face (grimaced or relaxed), Legs (curled or at rest), Activity level (at ease or tense), Crying (moaning or screaming), and Consolability (content or inconsolable). To use the scale, the provider makes careful observations on these five features, tallies up the points, and follows the chart to construct a reasonable depiction of the patient’s pain.
CRIES is another pain assessment tool, used primarily for infants. Similar to FLACC, CRIES charts 5 objective traits to help a provider determine their patient’s level of pain. For instance, to complete the “R” portion of the scale, providers denote whether their patient “requires oxygen,” which can indicate pain in babies.
How to Use a Pain Scale
If, at your next visit, a medical provider hands you a piece of paper depicting the Universal Pain Scale, don’t overthink it. Too often adults go into “analysis paralysis,” afraid to admit their pain is severe or worried they won’t be taken seriously if they choose a low number. Just be honest. The universal pain scale is imperfect, but its multifaceted design can help you feel confident in your selection.
In addition to the pain scale, your provider may ask you to elaborate on your pain. To give them a clear picture of what you’re experiencing, try using words such as “dull,” “shooting,” “throbbing,” “white-hot,” etc., to further characterize your pain.
Finally, remember that a pain scale is one tool among many that a provider uses to make a diagnosis. Depending on its severity, your answer may alert them to a problem and prompt further tests, or it may put them at ease and confirm their suspicions.

